Tibial Tubercle Osteotomy (TTO) and MPFL Reconstruction Surgery: Explained and Recovering Journey
- Jul 18, 2024
- 5 min read
Updated: Jun 23, 2025
By Romtin G.
Before reading this article, check out our Instagram page where we'll have infographics on each article topic. They're perfect if you want a short introduction before reading the article, or if you want to get a general idea of the topic without reading the entire post. Here's the infographic in case you want to see it on our website instead: Infographic 2
If you’d like more context on this post, I’d recommend reading my previous post “Patellar Dislocation: What’s Getting Relocated” to get a basic idea of the physiological mechanism behind a kneecap dislocation, different genetic risk factors, and what would lead to a surgery like this. I will also be talking about another, less invasive surgery that will happen at the same time as my main surgery – an MPFL reconstruction surgery.
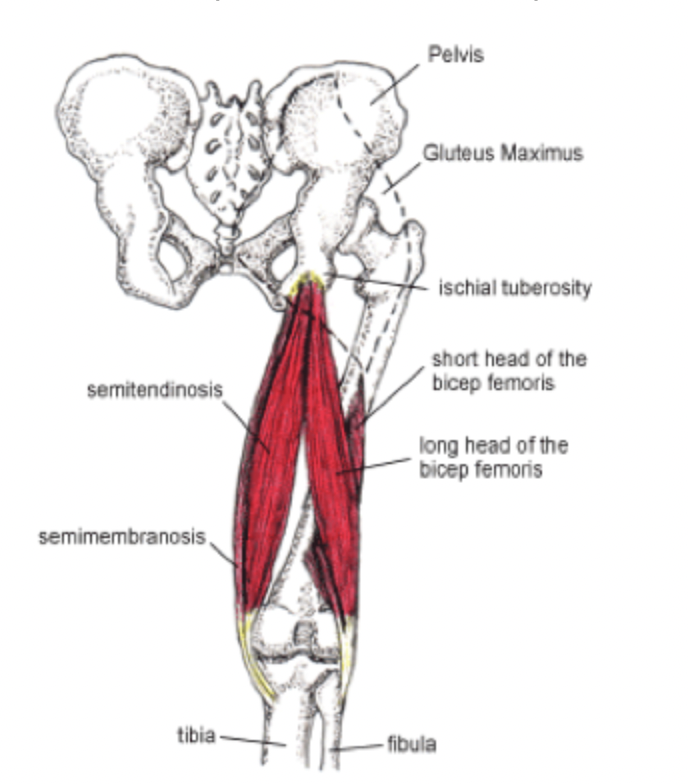
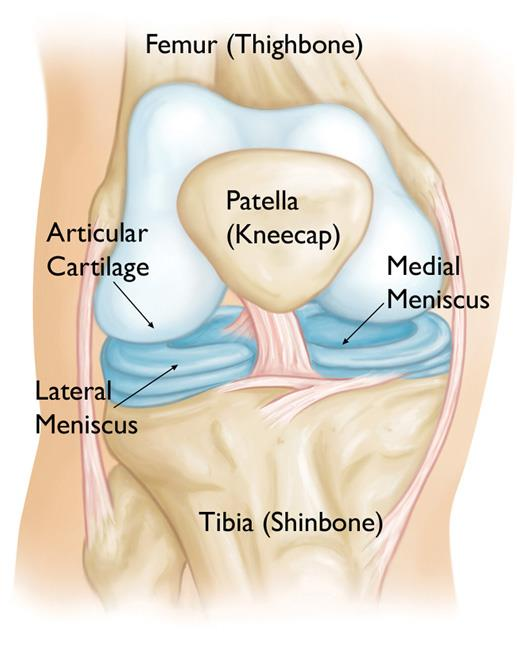
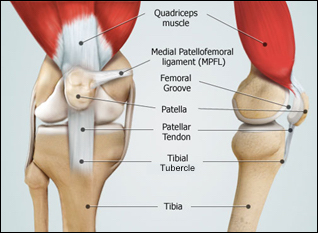
After multiple knee dislocations, surgery is often looked into for two main reasons: multiple dislocations indicate that there could be a genetic factor(s) (such as patella alta, trochlear dysplasia, or loose ligaments; read my first article to learn about these terms) at play, and further cartilage damage needs to be prevented. The TTO is to correct the kinesiology of the knee joint as much as possible by cutting and moving the tubercle to a new position so that the patella will function correctly, tracking and gliding smoothly across the trochlea (a part of the patellofemoral groove, where the kneecap sits). But what is the tibial tubercle? If you set your foot down so that your knee is perpendicular to the floor and run your finger from the center of your kneecap, you’ll sense a slight increase in elevation. Right where that increase happens is a small bone called the tibial tubercle (TT). It’s okay if it’s not that prominent for you – in fact, it’s normal for it to not be too visible. Osgood-Schlatter syndrome, mostly common in adolescents during growth spurts, results in a swollen and prominent tibial tubercle after certain activities, such as stair climbing or running. During a growth spurt, the quadriceps tendon (which connects the quadriceps to the knee) tightens, straining the growing TT, especially during physical activities that involve the contraction of the quadriceps. Anyways, the TT is the attachment site for the patellar tendon (the tendon that connects the tibial tubercle to the patella), allowing for the knee’s extensor movements like kicking, jumping, and walking. When the quadriceps contracts, it pulls on the patellar tendon, in turn pulling on the TT, and allowing for knee straightening.
TTO Surgery
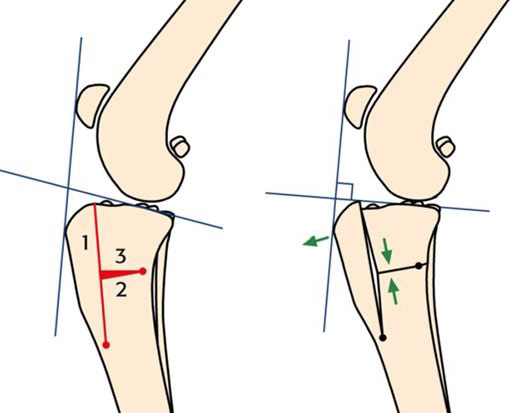
Okay, now we can get into the surgical procedure of the TTO. This surgery’s goal is to minimize the distance between the TT and the trochlear groove, allowing for a transfer of stress on the knee from areas of chondrosis (cartilage thinning) to areas of intact cartilage. After general anesthesia is administered, the surgery starts with a 6-10 cm longitudinal incision over the TT, starting just below the bottom of the patella and extending distally (away from the point of origin) along the tibia (shin bone). Then, the subcutaneous tissue (the layer of tissue underneath your skin) and fascia (connective tissue) are dissected carefully to expose the patellar tendon and the anterior surface of the tibia, making sure that a fat pad (something that helps to reduce friction between interior structures) known as the deep infrapatellar bursa is not damaged and that blood supply to the tendon persists. Then, using an osteotome (a type of saw), a horizontal cut is made through the TT at a predetermined level. The segment of the TT is mobilized carefully, maintaining attachments to the patellar tendon and surrounding soft tissues, and it’s shifted anteriorly or laterally, depending on the direction it was moved out of place due to injury. This segment is stabilized using screws that are placed through pre-drilled holes in the bone. Now, the actual movement is all done, and the wound needs to be cleaned with sterile saline to ensure cleanliness. Then, the deep fascia, subcutaneous tissue, and skin are respectively closed, using absorbable sutures for the deeper layers and non-absorbable sutures or staples for the skin. This surgery is pretty major, and I’ll be unconscious for about 2 hours until completion. But my journey doesn’t end there. For 6-8 weeks, I’ll have to be on crutches, which is crazy because during my first dislocation, I was on crutches for just a week and my armpits were already so sore! 9-12 months after surgery, I can return to regular activity with caution. It’ll take a long time to get to the point of full recovery, but it’s not impossible.
MPFL RECONSTRUCTION SURGERY
Briefly, I’ll also talk about the MPFL reconstruction surgery I mentioned earlier. As stated in my previous post, the MPFL is often damaged during a patellar dislocation, as the MPFL acts as a “leash” that restrains and controls the patella by keeping it within the patellofemoral groove. To prepare for the surgery, the patient is given general anesthesia, the knee is flexed up to 30 degrees to allow for easy access to the medial side of the knee, where the MPFL is located. A small incision is made on the medial side of the knee to access the MPFL, exposing the patella and the femur. Then, a graft (a piece of tissue) is prepared, which can be an autograft (the patient’s tissue) or an allograft (donor tissue). The donor is often a cadaver (a corpse), which is where I will be getting the tissue for my surgery! My surgeon did not want to take a graft from my tissue as he didn’t want to risk weakening other tendons, since grafts are commonly taken from the quadriceps tendon or the gracilis tendon. The surgeon then drills holes into the patella and the medial femoral epicondyle where the graft will be anchored, and then the graft is placed using BioComposite SwiveLock® Anchors and BioComposite FastThread™ Interference Screws, which provide biological integration and strong fixation. The next and most important step of the surgery is to tension the graft to replicate the natural tension of the MPFL. After injury, the MPFL will heal but never back to its original tensile state, so this step is crucial to restore the stability of the patella. Because this surgery will be happening at the same time as my TTO, the recovery phases interfere with each other, but if I had only done this surgery, I would be on crutches for the first two weeks, and then after 6-12 months, I would be able to return to full activity.
CONCLUSION
Finally, just as I did in my previous article, I’ll give a short recap of all I talked about. After having had multiple knee dislocations, surgery is often necessary to address genetic factors like patella alta or trochlear dysplasia and to prevent further cartilage damage. Tibial tubercle osteotomy (TTO) involves repositioning the tibial tubercle to correct patellar tracking and reduce stress on damaged cartilage areas, and MPFL reconstruction surgery repairs the medial patellofemoral ligament to stabilize the patella, often using a donor graft. Recovery from these procedures involves a lengthy rehabilitation period, intending to return to full activity within 9-12 months. I think for my next article, I’ll talk about another joint, so please leave recommendations down in the comments. If anyone has had any experience with surgery in general, please leave some comments down in the comment section to help me and other interested individuals out. Thanks for your time!
Sources: