Load, Lengthen, Snap! Hamstring Avulsions
- Aug 6, 2025
- 5 min read
Introduction
Most people have experienced a hamstring strain at some point, like during a sprint when you hear a “pop” in the muscles behind your knee and you limp off the track with an ice pack. But far fewer realize that the hamstring can actually rip completely off the bone! This severe injury, called a hamstring avulsion, is one of the most dramatic soft tissue (non-rigid tissue that supports the body’s muscles/organs) injuries in sports. It’s also one of the most biologically complicated, since it involves a lot of different tissue types, forces, and challenges in healing and regeneration. Beneath the surface of this tear lies a cool story of how muscle, tendon, and bone work together (and what happens when that relationship fails!!!).
Anatomy of the Hamstring
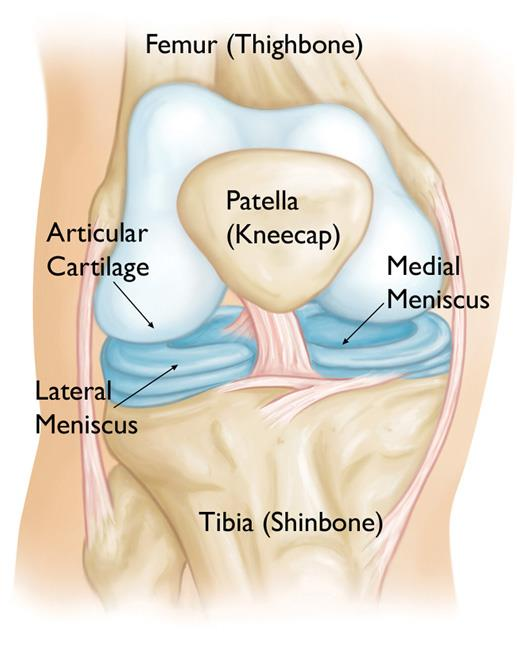
The hamstring is a muscle group that has three muscles: the biceps femoris, semitendinosus, and semimembranosus. The order they appear in your leg, from lateral (outside) to medial (inside), is biceps femoris, semitendinosus, and semimembranosus. In case it’s helpful to know, I use the phrase “Be The Man” to remember this order!
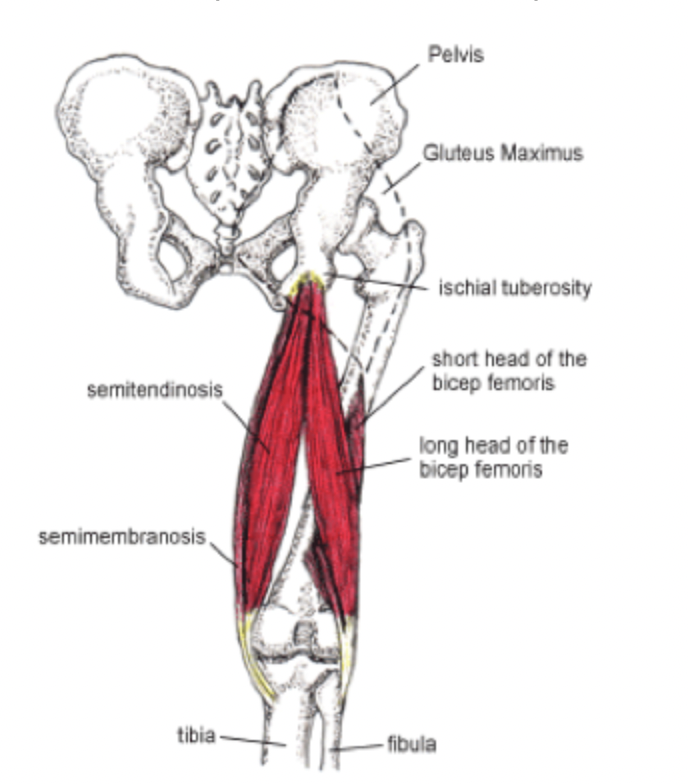
Anyways, they all originate at the ischial tuberosity, a bony ridge at the base of the pelvis, and cross behind the hip and the knee. Since they cross two joints (the hip and the knee), they act on two joints, which allows the hamstrings to both extend the hip and flex the knee. This is especially important when you’re doing activities like running, jumping, and lunging.
During sprinting, particularly in the late swing phase, the hamstrings contract to decelerate the forward motion of the lower leg. This phase causes the leg to experience extremely high tension, since the hamstrings are resisting the extension of the knee while the hip remains flexed. In these milliseconds of high mechanical demand, the hamstring is both contracting and lengthening (relaxing), creating the perfect storm for an injury!

Mechanism of Injury
Muscles are attached to bones via tendons (a type of connective tissue), and a typical hamstring strain involves small tears within the muscle belly (thick, contractile part of the muscle) or at the musculotendinous junction (where muscle transitions into tendon tissue). But in an avulsion, the injury occurs at the ischial tuberosity, which is the bone to which tendons of the hamstrings are anchored. The mechanism is almost always a sudden eccentric load (a force applied to an object that isn’t aligned with its center of gravity, causing it to bend/flex) during hip flexion and knee extension. For example, a hurdler might take off with their hip flexed and knee quickly extending. If the contraction force spikes high enough, the tendon can tear off part of the muscle and bone entirely.
Once detached, the muscle can snap upward like a released rubber band, bunching up in the upper thigh. In some cases, it even pulls off a small piece of bone along with it, especially in younger athletes who have incompletely fused growth plates. The result is a total loss of continuity between muscle and bone, which makes it impossible for the muscle to properly carry out its function.

Tissue Biology and Healing Challenges
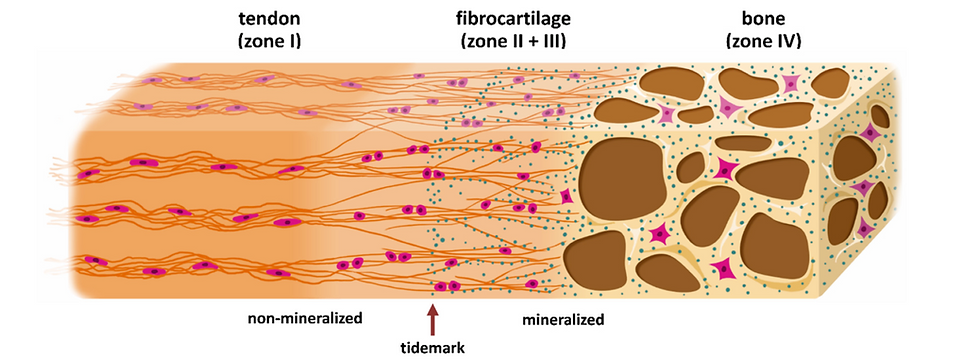
A hamstring avulsion is pretty difficult to heal because it involves three very different tissue types: bone, tendon, and muscle. Each has its own vascularity (blood supply), structural role, and regenerative potential.
Tendons are composed mostly of densely packed collagen fibers and have poor blood supply. This limits their ability to heal on their own, especially when completely torn away from their bony anchor. Without surgical reattachment, the tendon may scar over or fail to reconnect entirely, which could cause long-term weakness or muscle dysfunction.
The bone itself, if involved in an avulsion fracture, generally has better healing capacity, but only if the fragments are properly aligned. And muscle tissue, while more vascular and capable of regeneration, undergoes lots of necrosis (tissue death), inflammation, and scar formation when it retracts and loses attachment. Over time, the muscle fibers can shorten and atrophy, reducing both range of motion and strength.
What complicates matters even more is the nature of the tendon-bone junction, known as the enthesis. This transitional zone includes layers of fibrocartilage and mineralized tissue that gradually merge tendon into bone, and recreating this gradient after injury is super difficult. Current surgical techniques rely on suture anchors drilled into the bone, which can hold the tendon in place but may not perfectly mimic the original interface. That’s why bioengineering and materials science are so important! In these cases, we could design interfaces in the lab that replicate the gradual transition from tendon to bone and really improve healing outcomes and function restoration. Or, you could find a way to hijack the wound healing pathway to produce original, native tissue and not scar tissue (which can hinder treatment and is not as functional as native tissue).
Diagnosis and Clinical Presentation
Unlike a strain, which can vary in intensity and mostly resolves with rest and rehab, a hamstring avulsion is a more serious injury that normally requires surgical attention. Athletes often report a sudden, tearing pain during activity, followed by weakness, bruising, and difficulty walking or sitting. Sometimes, you can even see a noticeable dent or gap in the upper thigh where the tendon has pulled away.
Diagnosis is usually confirmed with MRI, which allows clinicians to assess the number of tendons involved, the degree of retraction, and whether there’s an associated bone fragment. Early diagnosis is super important, since after a few weeks, the window for easy surgical reattachment closes as the muscle retracts and scars.
Surgical and Non-Surgical Treatment
When the tendon is retracted more than two centimeters, or when multiple hamstring tendons are avulsed, surgical repair is the preferred option. During surgery, the tendon is pulled back into position and re-secured to the ischial tuberosity using suture anchors. Post-op care often involves a period of non-weight bearing, followed by progressive rehab focusing on range of motion, strengthening, and neuromuscular control.
In less severe cases (partial tears or minimal muscle retraction), non-surgical treatment may be possible. These rehab programs typically begin with rest and controlled movement, followed by eccentric strengthening exercises. However, outcomes are generally better with early surgical repair in complete avulsions, so if you feel hesitant about your case, it’s always best to talk with your healthcare team about which option would be best.
More About Rehab
One of the central challenges in rehab is reconditioning the hamstring to tolerate eccentric loading, which is the very motion that caused the injury. Exercises like Nordic hamstring curls are used to increase muscle length, tendon stiffness, and resistance to reinjury. It’s also important to retrain neuromuscular coordination. After injury, athletes often unconsciously shift their movement patterns, relying more on the glutes, lower back, or the uninjured leg. These compensations may protect the injured leg in the short term but increase the risk of secondary injuries if not corrected, so gait training, core stabilization, and proprioceptive drills are all important in a strong rehab plan.

What This Injury Teaches Us
Hamstring avulsions may be rare compared to strains, but they represent one of the best examples of how force, structure, and biology intersect. They expose the vulnerability of the tendon-bone interface, the limits of muscle tension, and the body’s patchy ability to recover from full structural failure.
For athletes, coaches, and clinicians, they’re a reminder that power without control is risky, and that the human body has its breaking points. For scientists and engineers, they offer a template for exploring better ways to reinforce soft tissue, improve surgical techniques, and design smarter rehab protocols.
Thank you for reading this article!
Sources