Surgery 2.0: Held Together by Hardware (Intramedullary Nailing of My Tibia)
- golabiromtin
- Apr 9, 2025
- 7 min read
Updated: Jun 23, 2025
By Romtin G.
Introduction and Pre-Surgery Experience
It’s been a long time since I’ve talked about my experience with surgery!!! Last Wednesday, April 2, I forgot my watch in chemistry because I took it off for a test. No big deal, right? So I jogged back for 10 seconds, and guess what? I heard and felt a SNAP. But this time, not in my knee. It was somewhere in my leg. I looked down and saw a huge deformity. My upper and lower legs looked like they were going in two different directions. Luckily, there was a bench nearby, so I just sat on it. Two friends happened to be passing by, and I asked them to get Mr. Melby and tell him to send the guy in the golf cart to take me to the office.
The school nurses were super kind and tried to keep my mood up, but I was thinking about all the wrong things. Even though my leg looked ugly and pulverized, my first thought was "My mom's gonna be super mad at me." Of course, I still called her, and she was rightfully upset once she knew I was "ok." It’s just that this whole process happening again so soon after the first surgery is stressful for both of us and has consequences that impact my whole family.
So what did we do? We went to UCSF Benioff Children’s Hospital in Oakland. Again. They took me in, triaged me, and another nice nurse named Aubrey rolled me into the ER room. Apparently, she had surgery on the exact same day as me (12/17/24) to remove her gallbladder! Around 8 PM, I was transferred to the third floor, which was a bigger, warmer room with a much nicer bed (the food still sucked). But there was a crying baby and a patient my age who just threw up his burrito. What an awesome hospital experience! That's what I remember most about the hospital because both my parents were just as upset as I was, and we were starting to plot against the baby. I thought the baby was crying on purpose because I swore I heard it start speaking English.
Anyway, it was time for surgery when I woke up the next day (Thursday). I was transferred to the fifth floor, met my surgeon, and went in for surgery that day. Honestly, it wasn't too bad. The nurses and doctors were funny, I got Vicodin, then anesthesia, and then I woke up in recovery with 13 pieces of hardware inside me.
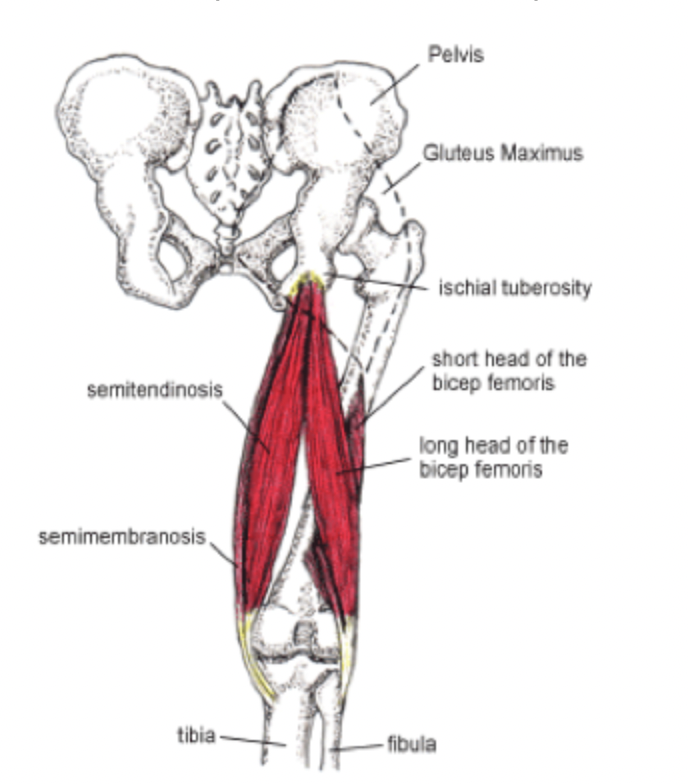
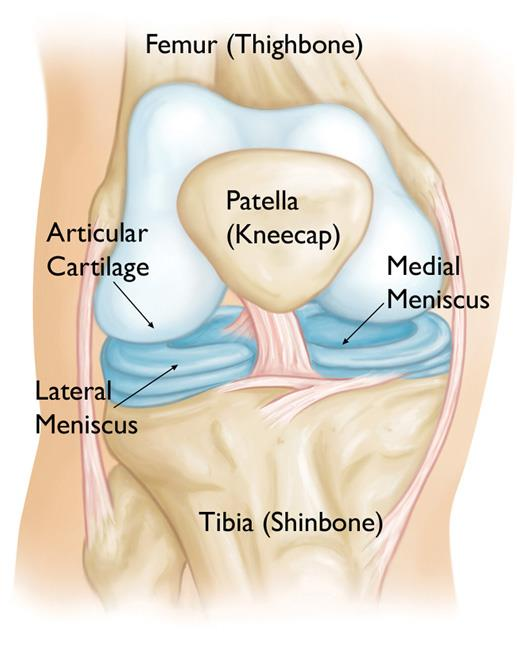
But what was the diagnosis? A left proximal tibia fracture that started along the line of the osteotomy cut from my Tibial Tubercle Osteotomy back in July (read my previous article linked here). It then branched and fractured around the screws and hardware they had placed earlier for this procedure. Below, I’ll show you X-rays of my knee fracture, but not the physical photos of my knee because they may be disturbing to look at. It’ll help you understand my description of the fracture. Keep in mind that the screws you see were from my previous surgery and have been removed as of now.


What I thought was the cut from my last surgery didn’t fully heal or strengthen the way it should’ve. X-rays might’ve looked “good enough,” but looks can be deceiving. The biomechanical stress from walking, stairs, and that tiny little jog likely re-directed force vectors straight to the vulnerable area — the tibial tubercle and nearby hardware. Or, the hardware itself may have weakened the nearby bone by taking most of the load (this is called stress shielding), and when the weakened bone had force directly applied, it just snapped. Maybe my body was just not used to the properly aligned tibia and didn’t know how to compromise and accommodate just yet. Another possibility: I had a whole lot of bad luck. Whatever the reason, what happened happened and I need to focus on recovery now and not injure my leg again. You can only do so many surgeries on the same limb!
Surgery Summary
Before I get into post-surgery, I want to walk you through what my actual surgical procedure was like. I was asleep (obviously) so what I’m saying is purely based on the talks I’ve had with my surgeon and the brief notes provided on the procedure.
They started off by sanitizing my skin with alcohol (provides an instant wipe-out of microbes) and chlorhexidine (a compound with a more long-term anti-microbial effect). They also made sure to confirm my identity, procedure site (the doctor used a sharpie to draw his signature on my left knee the night before!), and that I had received prophylactic antibiotics (Ancef) to reduce the chance of any infection.
The operation began with an incision along my previous scar over the proximal tibia and my kneecap. The surgical team dissected through layers of tissue to expose the site of the fracture, and by using a scalpel, curette, and rongeur, they cleaned the site of fibrous tissue and debris to ensure proper bone contact. Then, they put manual pressure to realign the proximal and distal fragments of my tibia. Once this alignment was confirmed with an x-ray, a mini fragment (mini frag) plate was fixed to the lateral side of my tibia with 2.5mm non-locking screws. This plate basically acts like an external splint inside my body and mechanically stabilizes the bone by holding the fragments in place as new bone forms across the fracture line. Two previous implanted screws (remnants from my TTO in December) were removed, while the tubercle osteotomy (the piece of bone that had been surgically moved in my TTO) was noted to be fully healed. This part surprised me because the fact that my bone was fully healed meant that there was actually an underlying problem that had nothing to do with my healing, pointing more toward the possibility that either the hardware or the realignment had changed the forces on my bone.
To further stabilize my tibia from within, the surgical team placed a ball-tip guide wire through the proximal tibial entry point down to the distal tibial physeal scar. The physeal scar is the band of bone that forms after the growth plate (physis) has fully fused, and the fact this was present means I am forever 5’7’’! They then reamed (enlarged) the inner canal of my tibia up to a diameter of 12mm, making space for a titanium intramedullary nail—an 11mm by 330mm rod that now lives inside the length of my bone. This nail essentially functions as an internal splint, bearing weight and ensuring proper alignment from the inside. Locking screws were then placed to secure the nail inside the bone. One screw was inserted from front to back near the top of the nail, followed by two diagonal (oblique) screws, and finally two screws near the bottom of the nail. These were guided into place using live X-ray imaging and a technique called the “perfect circle,” which helps surgeons line up the screws precisely and lock the nail in place to prevent it from twisting or shifting. These screws prevent the nail from shifting and keep the bone fragments tightly compressed—a critical factor for stimulating bone healing via Wolff’s Law, which states that bone adapts to the mechanical stresses placed upon it.
With the hardware in place, the wound was thoroughly irrigated and closed in layers with absorbable sutures for the deeper tissues and non-absorbable nylon in a vertical mattress configuration for the skin, promoting optimal healing. I was then transferred to the recovery room in stable condition, and I woke up to my parents sitting next to me. I now had a mini frag plate, 11 screws, and an intramedullary nail serving as both a scaffold and a stabilizer, holding me in place so my body can do what it does best—heal.
Post-Surgery Experience
Thanks to the nerve block, I didn’t feel much pain at first. I only needed one oxycodone pill in the night with Colace (a necessary stool-softener, since oxycodone can cause constipation), and I left the hospital Friday morning. Once I got home, though, the pain started creeping in. It wasn’t as horrific as the first surgery, but it was still rough. I manage it by taking Ibuprofen and Tylenol as needed, and I also take aspirin to help prevent blood clots in my leg.
Overall, I was feeling really weak and tired, and a part of this was due to the blood loss I had. I only lost around 100 mL of blood, which is considered minor in terms of the 5L of blood the average adult human has. But even that amount made me experience many of the symptoms of anemia, so my pediatrician recommended taking ferritin (a protein that stores iron within cells) tablets, and I’ve felt better ever since!
For a few days following my surgery (Saturday - Tuesday), I also had a low-grade fever. This initially worried me because I thought my wound was infected, which could lead to sepsis (a life-threatening overreaction to a pathogen) and would require immediate hospitalization. But then I realized that if I actually had sepsis, I wouldn’t be calmly overthinking it. I’d be in unbearable pain, crying my eyes out, and barely able to function. So, I did some research, and with an opinion from my doctor, I concluded that this was just a normal biological response. When the body undergoes severe trauma like surgery, the immune system launches an inflammatory response to protect against potential infection and begin tissue repair. This immune activation can trigger the release of pyrogens—molecules like interleukin-1 (IL-1) and tumor necrosis factor (TNF-alpha)—that travel to the brain’s hypothalamus and raise the body’s set-point temperature. The result is a mild fever (99º-100ºF or 37.2º-37.7ºC), which actually helps immune cells work more efficiently. In my case, this fever subsided within four days, with no signs of surgical site infection or other complications. It was just my body kicking into gear to heal and protect itself.
Conclusion
I know this article is very lengthy, but thanks for staying through to read it! The next article will most likely be on the stages of bone healing and different types of bone fractures. Hope you enjoyed this article!
Sources
None! All this information is from my own experience, my conversations with my attending care team at the hospital, and my ER Release Notes.