Understanding Spinal Injuries (Spondylosis)
- golabiromtin
- Jul 24, 2024
- 4 min read
Updated: Jun 23, 2025
By Romtin G.
Before reading this article, check out our Instagram page where we'll have infographics on each article topic. They're perfect if you want a short introduction before reading the article, or if you want to get a general idea of the topic without reading the entire post. Here's the infographic in case you want to see it on our website instead: Infographic 4
In this article, I’ll be talking less about the anatomy of the spine and more about the mechanisms and treatments for multiple different athletic and degenerative spinal injuries, following up on my previous article that gave you a general spine background. In case you decide to research these conditions on your own, you may encounter many terms that sound similar (as you will see soon). One term you should be familiar with before getting started is spondylosis, which refers to any spinal degenerative condition. It is not a single condition; it acts as an umbrella term for all kinds of spinal conditions, which will be elaborated on throughout this article.
I’ll start with two related injuries that both sound like the championship words in a spelling bee – spondylolysis and spondylolisthesis. Spondylolysis refers to a defect or stress fracture in the pars interarticularis, a small bony segment connecting the joints between and/or behind the vertebra in the lower back, particularly at the L5 vertebra (process of naming explained in previous article). It normally results

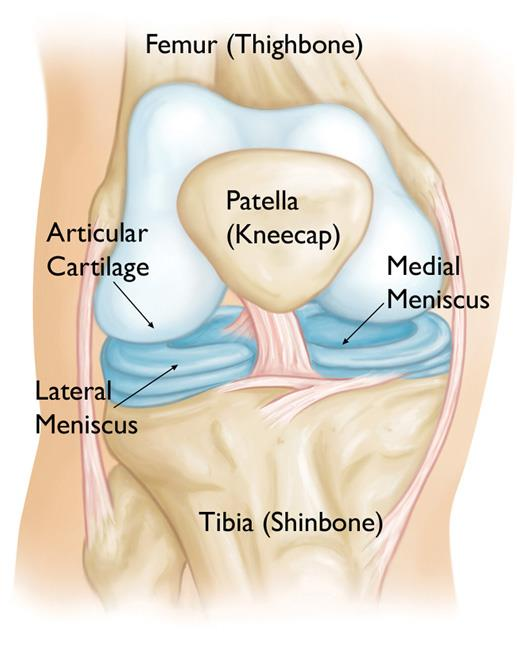
from repetitive stress and overuse, as the cartilage between the joints wear out and cause friction between vertebrae, a condition known as spinal osteoarthritis. This reduces mobility and increases friction between bones, leading to osteophytes (bone spurs) that can cause pain if they put pressure on surrounding spinal nerves, ligaments, or muscles.
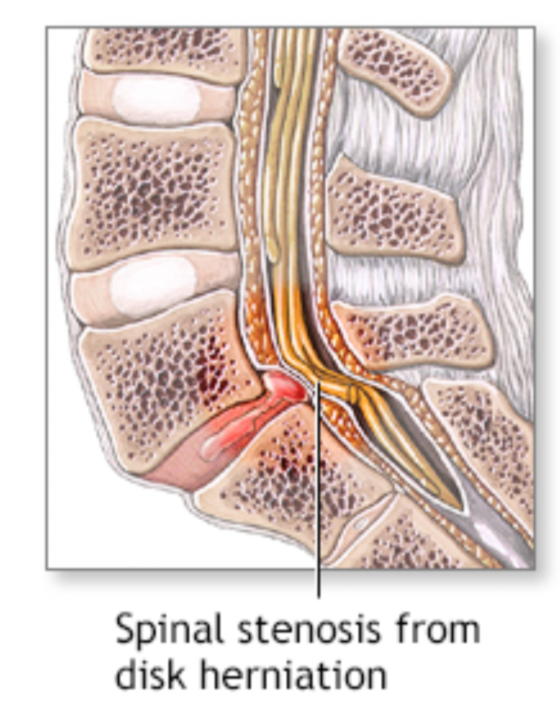
The development of bone spurs and other complications enlarges the joint, narrowing the spinal canal and compressing nerve roots, leading to a condition known as spinal stenosis where pain, weakness, and numbness presents itself in the affected area. Treatment plans for spinal stenosis and spondylolysis often follow with rest and activity modification, physical therapy, back brace (occasionally), non-steroidal anti-inflammatory drugs for pain relief, and surgery if conservative treatments fail. Recovery takes about 6-12 weeks, as long as the proper activity modification and physical therapy is followed.
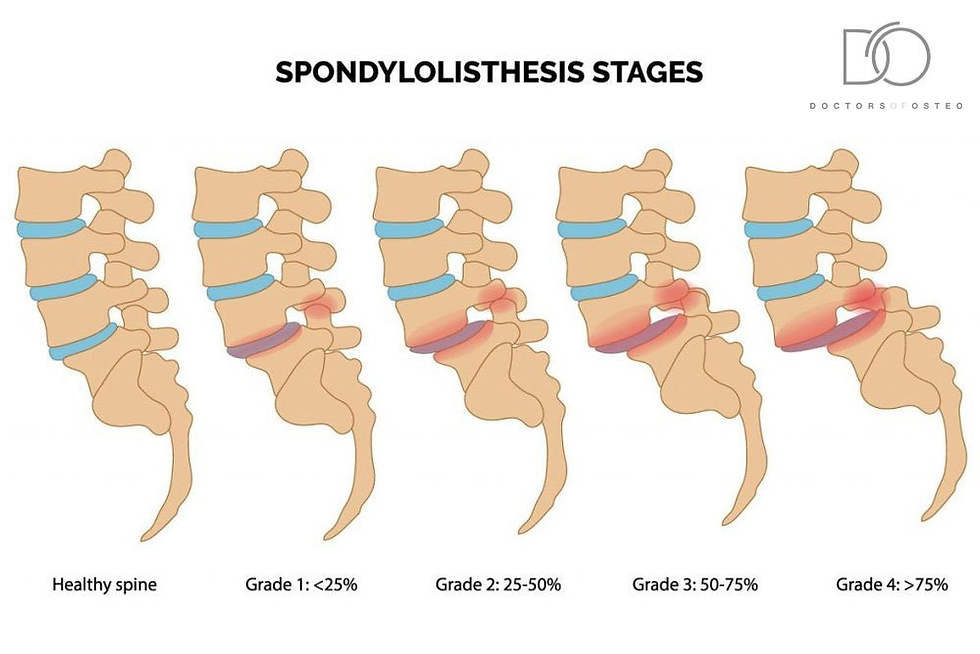
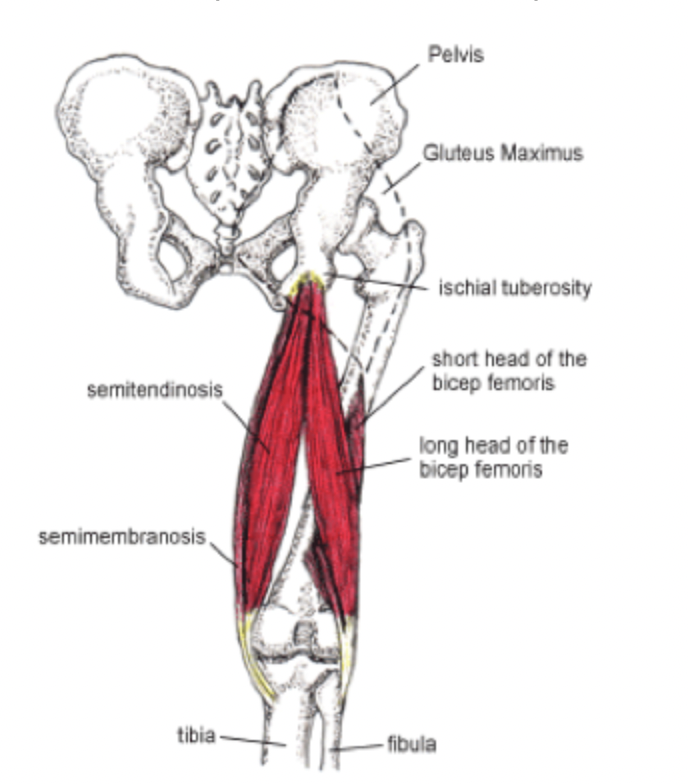
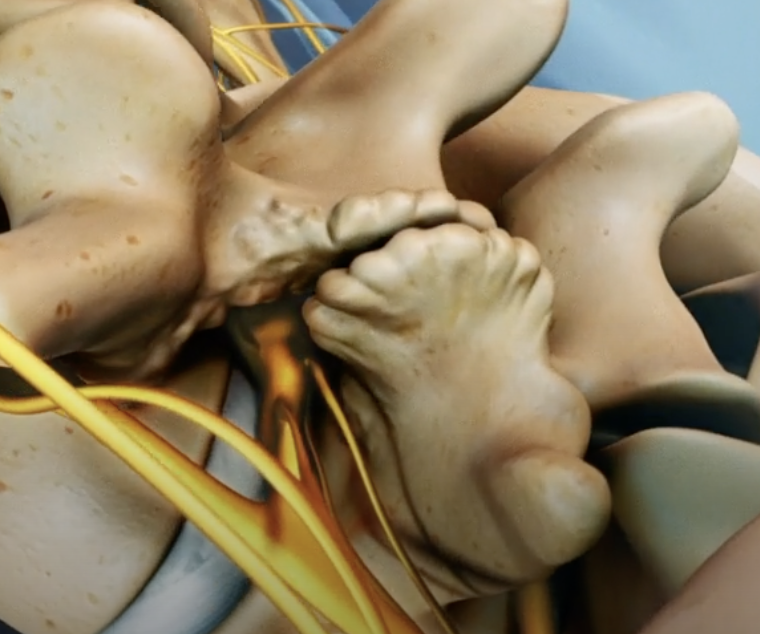
Spondylolisthesis occurs when a vertebra (commonly in the lumbar region) slips out of its proper position onto the vertebra below, often caused by spondylolysis, where the fracture weakens the bone and allows it to slip out of place. The slippage is classified in grades I-V in order of the severity and the amount of slippage. Grade I sponylolisthesis is 1 to 25% slippages, while Grade V is more than 100% slippages, a condition classified as spondyloptosis. Other causes include congenital defects (present from birth), trauma, or degenerative changes. Essentially, the slippage puts pressure on the spinal canal where the nerves extending from the spinal cord run through, resulting in lower back pain, radiating pain from the buttocks to the leg (similar to sciatica), muscles tightness in the hamstrings, and in severe cases, bowel or bladder dysfunction. This only occurs when significant vertebral slippage compresses a bundle of nerve roots at the base of the spinal cord called the cauda equina (leads to Cauda Equina Syndrome). The cauda equina controls the sensory and motor functions in the lower limbs and the pelvic organs, so compression of these nerves can lead to constipation, bowel incontinence, urinary retention, and/or frequent urination. Recovery efforts include rest, physical therapy, and epidural steroid injections to help with pain from pinched nerves. In severe cases like when one develops Cauda Equina Syndrome, surgery may be required to fuse the two vertebra so no more movement and damage occurs, to create space in the spine to relieve pressure on the nerves, or a combination of both.
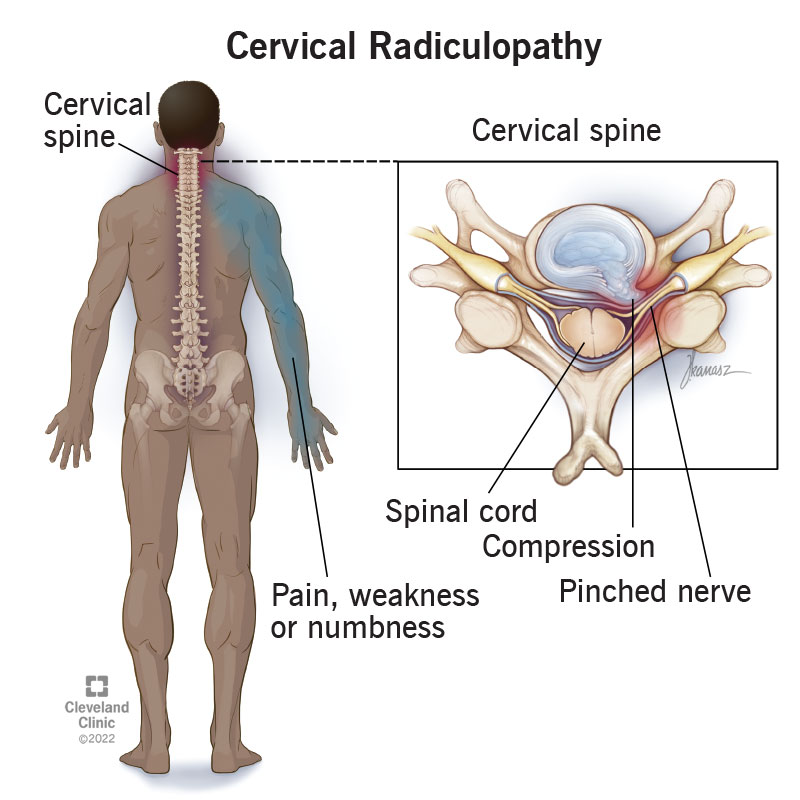
So far, I’ve talked about diseases that often affect the lower spine. But what about the upper spine? The last diseases I’ll discuss is called cervical radiculopathy, where the intervertebral disc(s) (shock absorber) in the cervical spine can rupture (another condition known as having a herniated disc), causing the inner gel-like center to put pressure against a nerve root in the cervical spine. This disease is more common in elderly people, because as people age, the cervical discs degenerate and lose height and elasticity. The degeneration increases the chance of disc herniation, cartilage breakdown, and the formation of bone spurs. This condition can also result from direct injury or trauma to the spine, such as from a car accident or sports injury, leading to disc herniation, fractures, or other conditions that compress nerve roots. The symptoms that follow with cervical radiculopathy include a sharp pain from the neck into the shoulder or arms (depending on the affected nerve), numbness or muscle weakness, and altered arm reflexes. Treatment involves physical therapy, pain medications, and ergonomic lifestyle adjustments (i.e., ensuring your chair has lumbar support and your feet are flat and perpendicular to the floor when you sit, keeping good posture, and taking regular breaks to stretch after sitting for 30-60 minutes). Surgery follows in severe cases, where the herniated disc is removed and replaced by a bone graft to promote fusion of nearby vertebrae.
Thank you for taking the time to read through this article. I hope you found the information both engaging and helpful, and if you have any further questions, feel free to reach out!
Sources:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/spondylolysis#:~:text=Spondylolysis%20is%20a%20stress%20fracture,out%20of%20every%2020%20people.